Procedure Selection
Basics
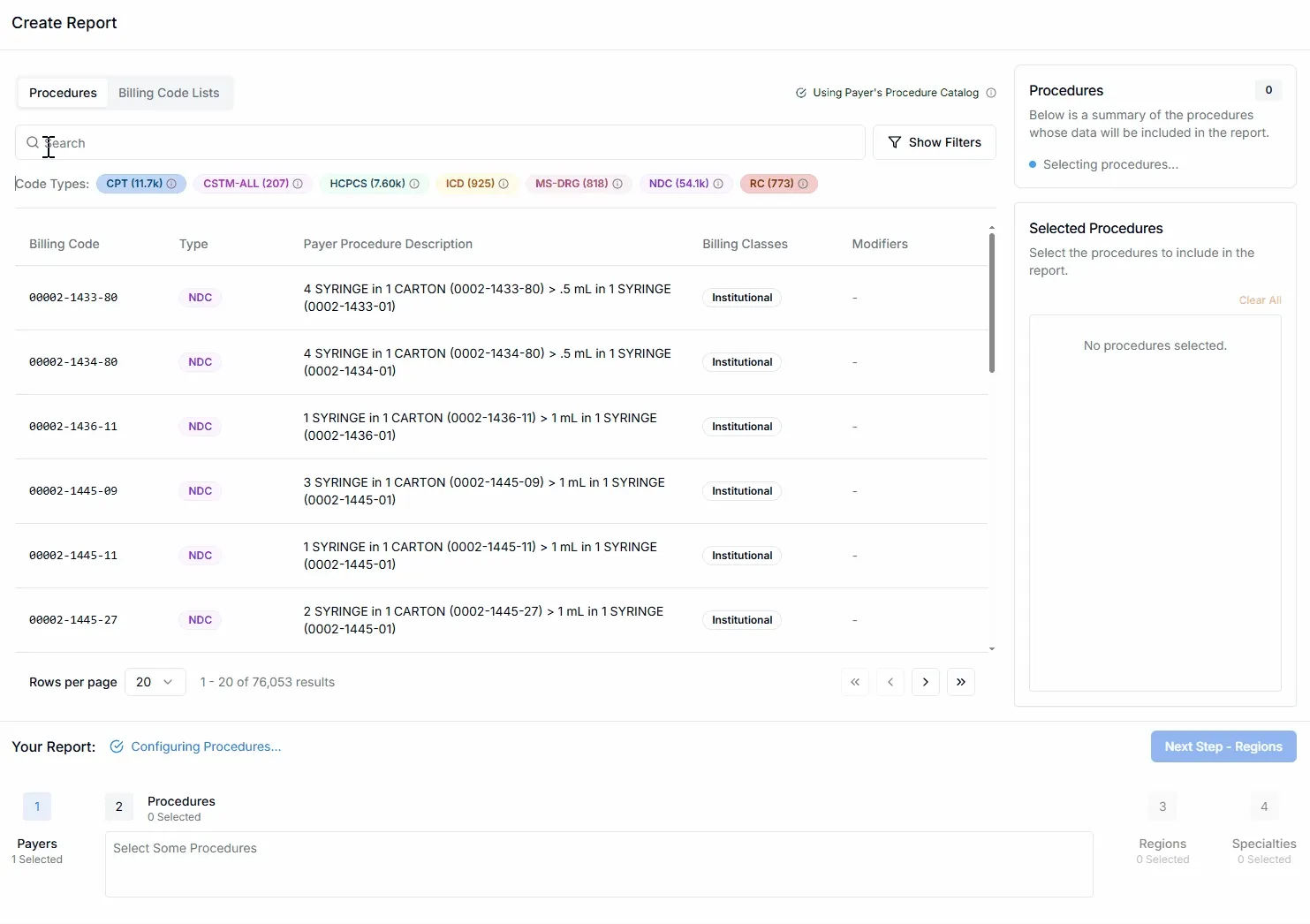
Select the medical billing codes for which you want to view reimbursements.
Use the search bar to lookup any alphanumeric medical billing code.
Not all payers negotiate rates for every single billing code code classification system or for every individual code within systems. Procedure Selector interfaces with PriceMedic’s Payer Data Catalogs to display a comprehensive breakdown of different types of billing codes included within the selected payer’s transparency data.
The Code Types list underneath the procedure search bar displays the count and category of all of the medical codes available to query for the payer you have selected. You can hover over each code type for a brief explanation of their typical usage.
Billing codes that match your search will be displayed in the table. Preview the payer’s procedure description, the billing classes associated with the code in the selected payer’s data (institutional or professional), as well as any billing code modifiers that the selected payer has associated with the billing code.
If you’ve saved Billing code lists specific to your organization, toggle to the Billing Code Lists tab at the top to select from them.
Add a billing code or list by clicking on its row in the table. Selected Procedures are displayed the right hand column You can remove a billing code by clicking the ❌ or Clear All within the Selected Procedures Section along the right hand side.
Select Next Step - Regions to proceed.
Billing Code Filters
Access filtering options for billing codes by selecting Show Filters to the right of the search bar.
Within the Filters pop-up you can pare down billing code search results based on the following requirements:
Billing Codes Types
Filter billing codes by their classification system, such as CPT, HCPCS, or ICD-10 codes.
| Code Type | Description |
|---|---|
| CPT | 5 digit numeric or alphanumeric codes maintained by the American Medical Association corresponding to the procedure or service rendered; also includes Proprietary Laboratory Analyses codes |
| CSTM-ALL & Local | Payer defined custom billing codes for the service or procedure described in the Payer Procedure Description field |
| HCPCS Level II | 4 digit alphanumeric codes designed to identify products, supplies, and services not included in the CPT system; HCPCS codes reference generic drugs only |
| ICD-10-CM | 3 digit alphanumeric codes to identify medical diagnoses and conditions based on classifications developed by the World Health Organization and modified by the National Center for Health Statistics |
| MS-DRG | 4 digit numeric codes developed by the Centers for Medicare and Medicaid Services to categorize and reimburse inpatient hospital services. Compare with APCs |
| APC | 4 digit numeric developed by the Centers Medicare and Medicaid Services in the United States to categorize and reimburse outpatient services provided by hospitals and other healthcare facilities such as Ambulatory Surgical Centers |
| NDC | 10 digit, 3 part numeric identifiers for all commercially distributed drug products maintained and assigned by the FDA; NDC codes are specific and unique to the labeler (manufacturer, distributor, or repackager), dosage and route, and formulation |
| RC | 4 or 5 digit alphanumeric codes maintained by the American Hospital Association to provide a broader classification of billable services such as Room and Board or Operating Room Services |
Billing Code Modifiers
Filter billing codes by additional two-digit codes that provide more information about the service or procedure.
| Modifier | Description |
|---|---|
| 22 | Increased procedural service |
| 23 | Unusual anesthesia |
| 24 | Unrelated E&M service during postoperative period |
| 25 | Significant, separately identifiable E&M service on the same day |
| 26 | Professional component |
| 27 | Multiple outpatient hospital E/M encounters on the same date |
| 32 | Mandated services |
| 33 | Preventive service |
| 47 | Anesthesia by surgeon |
| 50 | Bilateral procedure |
| 51 | Multiple procedures |
| 52 | Reduced services |
| 53 | Discontinued procedure |
| 54 | Surgical care only |
| 55 | Postoperative management only |
| 56 | Preoperative management only |
| 57 | Decision for surgery |
| 58 | Staged or related procedure during the postoperative period |
| 59 | Distinct procedural service |
| 62 | Two surgeons |
| 63 | Procedure performed on infants |
| 66 | Surgical team |
| 73 | Discontinued outpatient procedure prior to anesthesia |
| 74 | Discontinued outpatient procedure after anesthesia |
| 76 | Repeat procedure by same physician |
| 77 | Repeat procedure by another physician |
| 78 | Return to the operating room for a related procedure |
| 79 | Unrelated procedure by the same physician during postoperative period |
| 80 | Assistant surgeon |
| 81 | Minimum assistant surgeon |
| 82 | Assistant surgeon (when qualified resident unavailable) |
| 90 | Reference laboratory |
| 91 | Repeat clinical diagnostic laboratory test |
| 92 | Alternative laboratory platform testing |
| 95 | Synchronous telemedicine service |
| 96 | Habilitative services |
| 97 | Rehabilitative services |
| 99 | Multiple modifiers |
| AA | Anesthesia services performed personally by anesthesiologist |
| AD | Medical supervision by a physician: more than four procedures |
| AS | Assistant surgeon services provided by PA or advanced practice RN |
| CR | Catastrophe/disaster related |
| CT | Computed tomography services |
| EY | No physician or other licensed health care provider order |
| F1 | Left hand, second digit |
| F2 | Left hand, third digit |
| GC | Service performed in part by a resident under the direction of a teaching physician |
| GQ | Via asynchronous telecommunications system |
| GT | Via interactive audio and video telecommunication systems |
| GZ | Item or service expected to be denied as not reasonable and necessary |
| KX | Requirements specified in the medical policy have been met |
| LT | Left side |
| RT | Right side |
| RR | Rental |
| TC | Technical component |
| NU | New equipment purchase |
| UE | Used equipment purchase |
Negotiation Arrangements
Filter billing codes by how the payment is structured between the payer and provider.
| Arrangement | Description |
|---|---|
| Fee for service (ffs) | Negotiated dollar values the payer agrees to reimburse the provider for each billing code |
| Capitation | A fixed amount paid per patient by the payer to the provider (often Health Maintenance Organizations and Accountable Care Organizations) for a predetermined period of time, usually monthly, for the provider to provide all healthcare services required by the patient during the covered period |
| Bundle | An all-in negotiated reimbursement for related services or procedures that are typically performed together that may not equal the sum of the Fee-For-Service rates of all of the services or procedures included in the bundle. Example: a bundle could be used to bill for all of the procedures and services associated with a colonoscopy such as anesthesia, professional services, and post-anesthesia care |
Billing Classes
Filter billing codes by whether they apply to institutional settings, professional services, or both.
| Class | Description |
|---|---|
| Institutional | Billing codes that apply only to services rendered in hospitals, nursing homes, or ambulatory surgical centers. Also known as facility fees |
| Professional | Billing codes that apply only to services rendered by physicians or other health care professionals |
| Both | Codes payers have listed in association with both professional and institutional billing classes |
Negotiated Types
Filter billing codes by how the reimbursement amount is determined and calculated.
| Type | Description |
|---|---|
| Negotiated, Derived, and Fee Schedule | Negotiated, Derived, and Fee Schedule are used almost interchangeably according to the preference of the payer. In general, they all represent the total dollar amount to be remitted to the provider for a procedure or service through a combination contributions of the payer and patient |
| Percentage | Payer agrees to reimburse the provider the a percentage of their billed charge or charged amount |
| Per Diem | Represents the negotiated daily rate to be reimbursed to the provider usually for ongoing services such as an inpatient or rehabilitation care |